Drug Repurposing Provides Big Impact for Patients
C-Path’s CDRC is positioned to inform future clinical trials for diseases of high unmet medical need with real-world clinical outcome data
By Claire Bessetti
 Millions of patients struggle every day with diseases that lack adequate treatment options. For many rare and orphan diseases, approved therapies are either absent or unsatisfactory, and healthcare providers may need to use existing drugs in novel ways for patients with difficult-to-treat conditions. Critical Path Institute’s (C-Path) CURE Drug Repurposing Collaboratory (CDRC) and the U.S. Food and Drug Administration’s (FDA) CURE ID app are expanding beyond infectious diseases into the realm of rare disease. With such expansion, it is important to highlight some incredible individuals who are true examples of how drug repurposing is advancing treatment options in areas of high unmet medical need.
Millions of patients struggle every day with diseases that lack adequate treatment options. For many rare and orphan diseases, approved therapies are either absent or unsatisfactory, and healthcare providers may need to use existing drugs in novel ways for patients with difficult-to-treat conditions. Critical Path Institute’s (C-Path) CURE Drug Repurposing Collaboratory (CDRC) and the U.S. Food and Drug Administration’s (FDA) CURE ID app are expanding beyond infectious diseases into the realm of rare disease. With such expansion, it is important to highlight some incredible individuals who are true examples of how drug repurposing is advancing treatment options in areas of high unmet medical need.
CDRC works closely with rare disease collaborators, including two professionals on the research and development side of drug repurposing.
 Shira Strongin
Shira Strongin
A bright, intelligent, beautiful woman is the first impression you get from Shira Strongin. You would never imagine the battles she has endured to still be alive. Shira has proven herself to be incredibly resilient, since she has had to relearn many basic functions, such as walking, reading, writing and speaking, due to many neurovascular events (e.g., strokes). She actively uses her experience to advocate for others.
Shira began experiencing odd symptoms as a child that signaled something was wrong. Her temperature readings were never normal, and she would often get sick for longer periods, compared to her classmates. These were easy enough to dismiss, but eventually more symptoms presented and their severity was no longer something that could be ignored.
Some of Shira’s experiences were particularly complex, including getting abnormal blood clots, despite her bleeding disorder, in which her platelets lack the ability to clot properly. Despite seeking care from experts around the country, there is still limited understanding of Shira’s underlying disease.
Approximately 8% of rare disease patients have approved therapies; Shira is in the 92% without any approved therapies. To control the condition, Shira has had to rely on off-label medications, as well as experimental agents. Her journey has included a lot of different treatments through trial-and-error, which have also resulted in significant side effects. These side effects were even severe enough to require hospitalization. This highlights the value of drug repurposing. Shira believes the reward can be enormous, as evidenced by her own survival. “I would not be alive if it were not for drug repurposing. This has caused me to be enthusiastic about drug repurposing and the impact it can have on rare disease patients’ lives,” Strongin says. She believes that treatment and survival should not be a privilege, but a priority for all. Therefore, we need to have programs that mitigate the risk and maximize the likelihood of success, like CURE ID and CDRC.
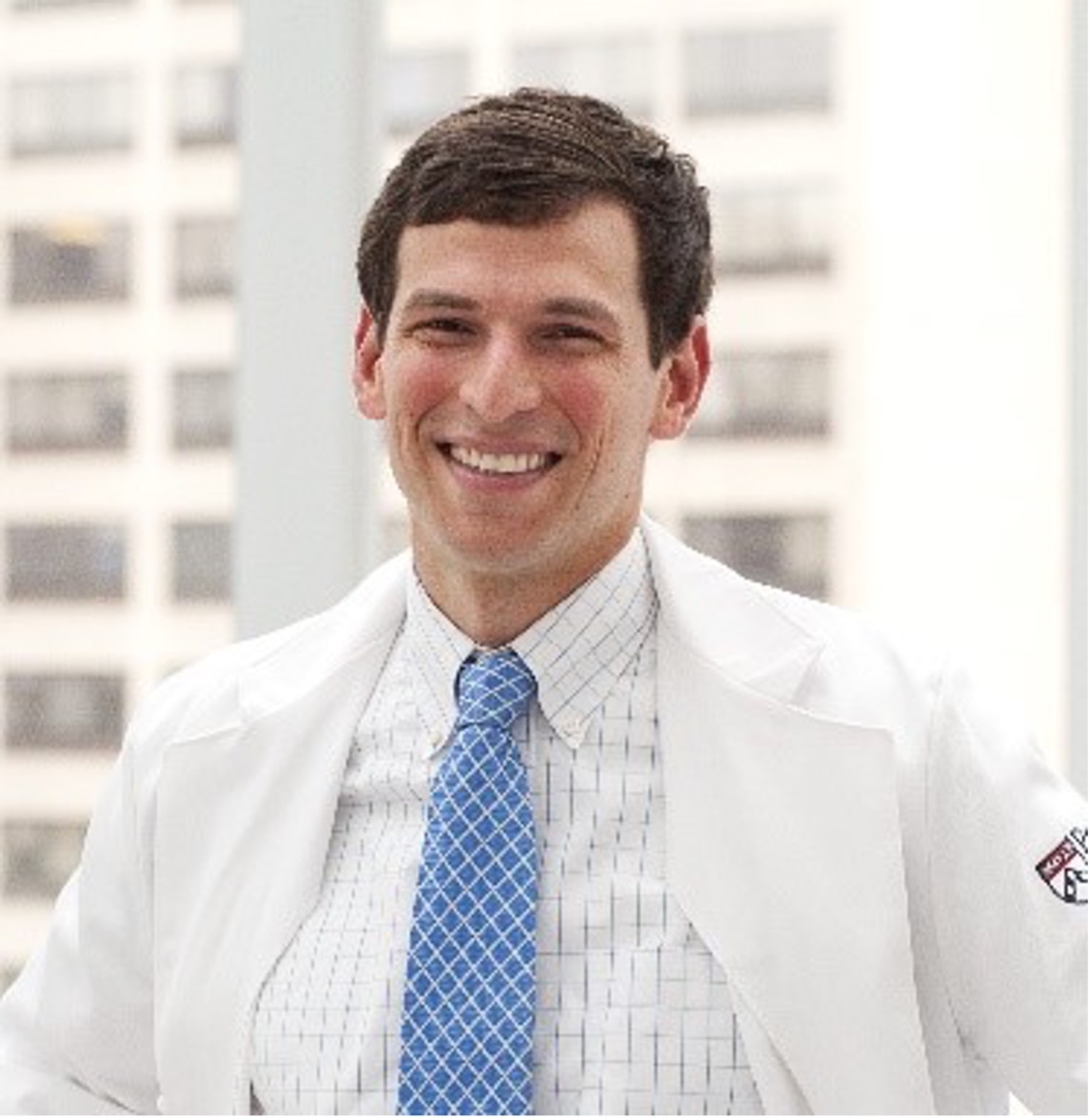 David Fajgenbaum, M.D., M.S., MBA
David Fajgenbaum, M.D., M.S., MBA
Dr. David Fajgenbaum is not afraid to think outside the box and that is what saved his life. While in medical school, the former college athlete suddenly became critically ill. Doctors told him he was suffering from a rare disorder called Castleman disease; his immune system was attacking his vital organs, potentially leading to life-threatening organ failure. He spent months in the ICU and at one point was read his last rites.
Then there was a turning point. After studying his own charts and testing samples of his own blood, David identified an unusual pattern in his bloodwork. With this piece of information in hand, he was able to look for drugs that acted on the elevated pathway, and discovered a drug used to treat another illness seemed to help him. David repurposed the kidney transplant drug sirolimus eight years ago to save his own life.
He tried the drug after connecting insights from his own samples with information from medical literature, though it hadn’t been studied in his disease. Finally, there was a breakthrough in his progress and Fajgenbaum has now been in remission for more than eight years.
David has gone on to create Every Cure, a nonprofit, human-centered, data-driven hub that accelerates connections between drugs and the diseases that they have the capacity to cure (1). The nonprofit is based on the concept that every drug on the market has multiple effects on the body, not just the one or two that first earned its approval.
“If we can do this for Castleman, if we can do it for cancer and if we can do it for COVID, there are a lot of patients out there waiting for solutions, we are going to do it across drugs and diseases,” Fajgenbaum said in an ABC interview (2). He thinks there are roughly 3,000 drugs out there that aren’t being fully utilized, but through Every Cure, he and his team hope to change that. “The idea here is how many more of these cures are just hiding in plain sight that we can unlock and save lives,” Fajgenbaum said (3).
What’s Next for the CDRC?
@CPathInstitute’ CDRC is positioned to inform future clinical trials for diseases of high unmet medical need with real-world clinical outcome data. For Clinical trial information visit our CURE ID App @id_cure. #ClinicalTrials #RealWorldData #RareDisease #PatientImpact
The CURE Drug Repurposing Collaboratory is committed to expanding the CURE ID app to include other diseases including rare diseases, rare cancers and ultrarare cancers. For rare diseases, CDRC is working on a group of genetic conditions known as RASopathies caused by mutations that alter the proteins in a particular molecular pathway known as Ras/MAPK. There are approximately 7-8 distinct RASopathy subtypes with NF1 being the most studied and most well-known. However, the remainder are much rarer and have limited financial interest from industry.
For rare cancers and ultrarare cancers, CDRC is working on a particularly problematic cancer known as sarcoma which begins in bone or in the soft tissues of the body, including cartilage, fat, muscle, blood vessels, fibrous tissue, or other connective or supportive tissue. Its rarity also makes it very difficult to standardize treatment as the disease is heterogeneous and consequently nearly impossible to study in clinical trials.
In collaboration with clinical sarcoma experts, patients, caregivers and patient advocates, the CDRC team has now finalized Clinical Case Report Forms (CCRF) for angiosarcoma, perivascular epithelioid cell tumor (PEComa) and epithelioid hemangioendothelioma. Additionally, C-Path’s CDRC team also finalized a CCRF for RASopathies in collaboration with clinical experts from the U.S., Canada and Europe. All its CCRFs were reviewed and accepted by the FDA.
Stay tuned for the updates and expansions that are brought to CURE ID and the CDRC.